Cholecystitis fasting from food and drink is a crucial component in the management of this inflammatory condition of the gallbladder. Understanding the rationale and guidelines for fasting can significantly improve patient outcomes and facilitate a successful recovery.
Fasting plays a pivotal role in reducing gallbladder activity and inflammation, alleviating pain, and promoting healing. This article delves into the pathophysiology of cholecystitis, the role of fasting in its management, and provides practical guidance for patients undergoing this therapeutic intervention.
Cholecystitis Fasting: A Comprehensive Guide: Cholecystitis Fasting From Food And Drink
Cholecystitis, inflammation of the gallbladder, is a common condition that can cause severe pain and discomfort. Fasting is an essential part of the management of cholecystitis, as it helps reduce gallbladder activity and inflammation.
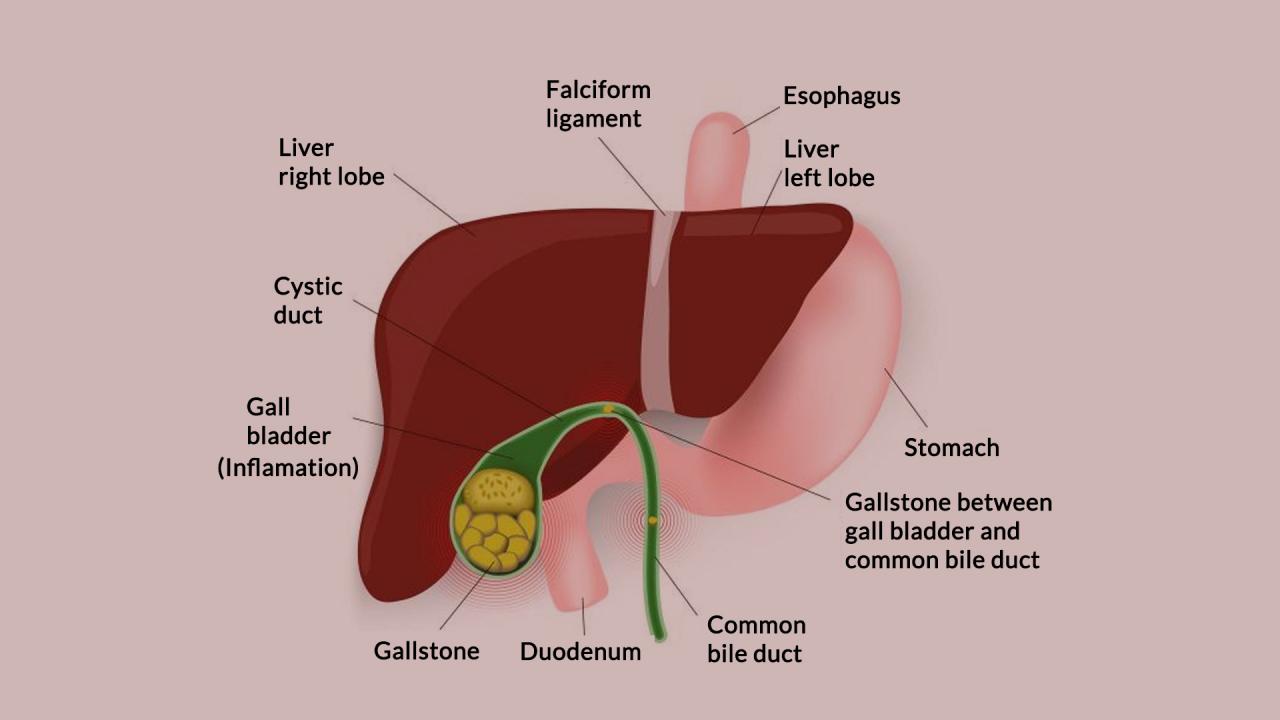
Pathophysiology of Cholecystitis
Cholecystitis is typically caused by a blockage of the cystic duct, which prevents bile from draining from the gallbladder. This can lead to bile stasis, which creates a favorable environment for bacterial growth and inflammation.
Jamaica’s culinary landscape boasts a vibrant blend of flavors and aromas, offering a tantalizing glimpse into the island’s rich culture. From the savory delights of jerk chicken and ackee and saltfish to the refreshing sweetness of tropical fruits, Jamaican food and drink is a culinary adventure that tantalizes the taste buds and leaves visitors yearning for more.
The inflammatory process involves the release of cytokines and other inflammatory mediators, which cause swelling, redness, and pain. If left untreated, cholecystitis can lead to serious complications, such as perforation of the gallbladder, sepsis, and even death.
Role of Fasting in Cholecystitis
Fasting is an essential part of the management of cholecystitis. By avoiding food and drink, the gallbladder is allowed to rest and inflammation can subside.
Fasting helps reduce gallbladder activity by decreasing the production of bile. This reduces the pressure within the gallbladder and helps to alleviate pain and inflammation.
Guidelines for Fasting
The duration of fasting required for cholecystitis typically ranges from 24 to 48 hours. During this time, patients should avoid all food and drink, including water.
Jamaica boasts a rich culinary heritage that reflects its diverse cultural influences. Jamaican food and drink are characterized by their bold flavors and vibrant colors, with a heavy emphasis on fresh, local ingredients. Ackee and saltfish, a national dish, is a savory breakfast staple, while jerk chicken and curry goat are popular lunchtime favorites.
For a sweet treat, try the famous Blue Mountain coffee or the delectable rum cake.
Exceptions may be made for patients who are unable to tolerate fasting, such as those with diabetes or other medical conditions. In these cases, a modified fasting regimen may be prescribed.
Monitoring and Management during Fasting, Cholecystitis fasting from food and drink
Patients who are fasting for cholecystitis should be closely monitored for signs of dehydration and electrolyte imbalance. Intravenous fluids may be necessary to maintain hydration.
Pain management is also an important part of fasting for cholecystitis. Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can be used to relieve pain and inflammation.
Alternative Therapies and Adjunctive Measures
In addition to fasting, there are a number of alternative therapies and adjunctive measures that may be helpful in the management of cholecystitis.
- Herbal remedies:Some herbal remedies, such as dandelion root and turmeric, have been shown to have anti-inflammatory properties that may help reduce gallbladder pain and inflammation.
- Heat therapy:Applying a warm compress to the abdomen can help to relax the muscles and relieve pain.
- Massage:Gentle massage of the abdomen can help to improve circulation and reduce pain.
Patient Education and Counseling
Patient education is an important part of the management of cholecystitis. Patients should be provided with clear instructions on fasting and other aspects of their care.
Patients should also be educated on the signs and symptoms of complications, such as fever, chills, and severe abdominal pain. They should be advised to seek medical attention immediately if they experience any of these symptoms.
Ultimate Conclusion
Fasting for cholecystitis is a multifaceted approach that requires careful monitoring and adherence to specific guidelines. By understanding the underlying principles and following the recommended protocols, patients can optimize their recovery and prevent potential complications. This article serves as a comprehensive resource for healthcare professionals and patients seeking in-depth information about cholecystitis fasting.
