Pancreatitis fasting from food and drink plays a crucial role in the management of this debilitating condition. This comprehensive guide delves into the rationale, types, and monitoring of fasting in pancreatitis, exploring the nutritional considerations and potential complications associated with this therapeutic approach.
Fasting in pancreatitis aims to reduce the workload of the pancreas, allowing it to rest and recover. Different types of fasting, such as nil per os (NPO) and clear liquid diets, are employed depending on the severity of the condition.
As the leaves begin to turn and the temperatures drop, it’s time to start thinking about plus size fall fashion . This season, there are plenty of stylish and comfortable options to choose from. From cozy sweaters to chic dresses, there’s something for everyone.
Understanding Pancreatitis

Pancreatitis is an inflammation of the pancreas, a small organ located behind the stomach that produces digestive enzymes and hormones. It can be either acute (sudden and severe) or chronic (long-lasting and progressive).
Causes
- Gallstones
- Alcohol abuse
- Hypertriglyceridemia (high levels of triglycerides in the blood)
- Autoimmune disorders
- Medications
- Trauma
Types
- Acute pancreatitis:Typically lasts for a few days and resolves with treatment.
- Chronic pancreatitis:Can cause permanent damage to the pancreas and lead to complications such as diabetes and malnutrition.
Symptoms
- Abdominal pain
- Nausea and vomiting
- Fever
- Jaundice (yellowing of the skin and eyes)
- Rapid heart rate
- Low blood pressure
Complications
- Pancreatic necrosis (death of pancreatic tissue)
- Pancreatic abscess
- Pseudocyst formation
- Respiratory failure
- Kidney failure
Fasting in Pancreatitis Management: Pancreatitis Fasting From Food And Drink

Fasting is a key component in the treatment of pancreatitis. It helps reduce inflammation and give the pancreas time to rest and heal.
As the temperatures start to dip, it’s time to start thinking about updating your wardrobe for fall. For plus-size women, finding stylish and flattering clothing can be a challenge. But this season, there are plenty of plus size fall fashion options to choose from.
From cozy sweaters and leggings to chic dresses and skirts, there’s something for every style.
Rationale
Fasting reduces the production of digestive enzymes, which can further irritate the pancreas and worsen inflammation.
Types of Fasting
- Nil per os (NPO):No food or drink by mouth.
- Clear liquids:Liquids such as water, broth, and tea that do not contain any solids.
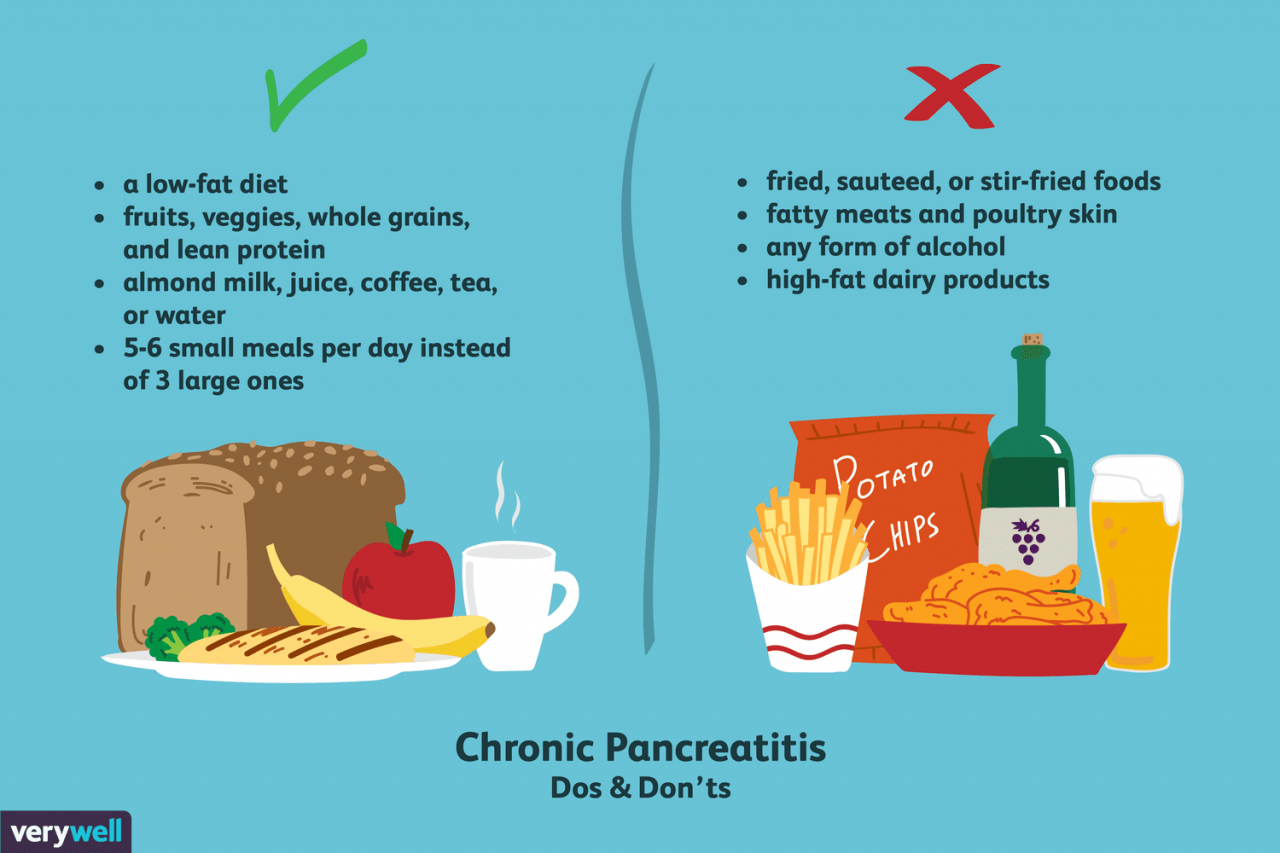
- Low-fat diet:A diet that contains less than 30% fat.
Duration and Monitoring
The duration of fasting depends on the severity of the pancreatitis. Patients with acute pancreatitis typically fast for 2-3 days, while those with chronic pancreatitis may need to fast for longer periods.
During fasting, patients are closely monitored for signs of dehydration and electrolyte imbalance.
Nutritional Considerations
Patients with pancreatitis have increased nutritional needs due to inflammation and reduced food intake. It is important to provide adequate hydration and electrolytes during fasting.
Hydration, Pancreatitis fasting from food and drink
Patients should drink plenty of fluids, such as water or clear liquids, to prevent dehydration.
Electrolytes
Fasting can lead to electrolyte imbalance. Patients may need to receive electrolyte supplements, such as potassium and magnesium.
Reintroducing Food and Drink
Food and drink are gradually reintroduced into the diet once the pancreatitis has improved. The diet should be low in fat and easy to digest.
Monitoring and Management
Patients with pancreatitis are closely monitored during fasting. Clinical parameters such as vital signs, blood sugar, and electrolyte levels are checked regularly.
Criteria for Discontinuing Fasting
- Resolution of abdominal pain
- Normal blood sugar levels
- Stable electrolyte levels
- Absence of complications
Potential Complications
- Dehydration
- Electrolyte imbalance
- Hypoglycemia (low blood sugar)
- Nutritional deficiencies
These complications can be managed with appropriate medical treatment and monitoring.
Concluding Remarks
Monitoring during fasting is essential to ensure adequate hydration, electrolyte balance, and timely resumption of oral intake. Potential complications, such as malnutrition and dehydration, should be promptly addressed to optimize patient outcomes.

